Dr. Pate’s Prescription for Change
St. Luke’s Dr. Pate on 2025 and the changing care ecosystem
Editor’s note: This is the second of a two-part series.
In the first part of this short series, I shared an environmental assessment as we prepare to develop our Strategy 2025. Here, I’m sharing thoughts about how the health care ecosystem is changing and will change over the next seven years.
Let’s start with insurance companies. There are a number of changes occurring in the insurance industry.
First, we can look at Oscar. This company is differentiating itself by focusing on the user experience, especially through the use of technology. Oscar offers its members free telehealth services and concierge “care guides” to help direct patients to high-value care. Oscar is finding success by partnering with the highest quality, highest brand preference health systems in each market it enters and offering its members narrow networks at a lower price than open access networks.
With a completely different strategy, CVS is acquiring Aetna and Walmart is acquiring Humana. Here, there seems to be a retail emphasis and the capability to drive members to retail health services at CVS and Walmart clinics. CVS and Walmart receive value when shoppers using their pharmacies spend time and money in their stores.
Still another strategy is that used by Optum (a subsidiary of UnitedHealth Group) and other national and local insurance companies that are getting into the provider side of the business. Optum now has more employed physicians than does Kaiser Permanente. The question will be whether insurance companies can lower the total cost of care spend through a focus on unit cost better than health systems can through a focus on integrated care and care management.
As it stands, 12 percent of employers offer defined contribution health plans for their employees, meaning that they give their employees a fixed amount of money that can be used to purchase a health plan. Generally, the employee can choose from a selection of health plans, but they are responsible for the costs above what the employer contributes. It is estimated that another 36 percent of employers are considering switching from defined benefit plans to defined contribution plans, not now while the labor market is tight, but in the next few years when we experience an economic downturn. Some of these employers will offer their employees a private exchange of health plans to select from, analogous to the public exchanges that uninsured individuals use to select a health plan.
Now let’s look at physicians. Again, we are seeing very different strategies. Among independent physicians, we are seeing direct primary care – a membership model where, in exchange for a membership fee, clinic visits are at no additional cost, the physician spends more time with you and certain basic services are included or provided a la carte for fixed fees that are transparent. This would not obviate the need for individuals to have health insurance; this benefit comes at an extra cost over and above the benefits the individual would already have. Nevertheless, there is a consumer segment that is willing to pay extra for improved access to and more time with physicians.
Within health systems, there has been a movement to primary care medical homes. These models require a great deal of investment and a lot of work on the part of the physicians and care team, but they seem to reduce costs for medically complex patients. The added benefit of primary care physicians within health systems is that they generally are on the same electronic health record as the specialists in that health system, resulting in better sharing of information among these physicians.
In some parts of the country, primary care companies have emerged that focus on the management of Medicare Advantage patients. They want to manage risk for this population only and have designed their processes to coordinate care and effectively manage this population.
Finally, let’s turn to hospitals. One of my colleagues recently stated that his job was to close all of his system’s hospitals, the implication being that hospitals will become a thing of the past and that with better care management, his system would be able to keep patients out of the hospital.
In a recent blog piece about the future of hospitals, I indicated disagreement with this position. Hospitals are not going away, though lower-acuity care will continue to move out of hospitals, even into homes with remote patient monitoring.
In the future, admissions to the hospital will be examined with root-cause analysis to determine where the system failed the patient. That is not to say that all hospitalizations can be prevented – I do not believe that. However, organizations like St. Luke’s Health System will learn from those cases where the admission could have been prevented and make changes to become ever more high performing. As a consequence, hospital utilization would be expected to decline.
The outlook for standalone rural, critical access hospitals looks bleak. There are at least three bills right now in Congress to provide improved reimbursement to enable these hospitals to become “outpatient hospitals,” that is to say, free-standing emergency rooms and primary care offices with lab and imaging services, but no inpatient beds. We have already experienced a significant number of rural hospital closures, and these bills are intended to stem this tide.
On the other hand, I think that the outlook for rural hospitals that are part of a system like St. Luke’s Health System is very good. We anticipate that more patients will be able to remain in their local hospitals for care through the use of telehealth services that will provide virtual access to specialists. There also will be patients who require care at our flagship hospitals who are not ready to go home, but who can be safely transferred to their local rural hospital for continued recovery. This would allow part of their hospital stay to be provided in a lower-cost setting.
What about microhospitals, those small facilities that are advertised as hospitals, but typically consist of an emergency room and a small number of inpatient beds? Most patients come in to the emergency room with conditions that could be taken care of in a lower-cost urgent care setting, are seen and treated, and released home within hours. Very few patients are admitted overnight, usually to receive IV fluids and medications. More complex patients have to be transferred to other facilities that are true hospitals and have the capabilities to manage serious illness.
I view these microhospitals as glorified urgent care centers, billed as much more expensive hospital services. At a time when health care systems are having to choose whether to ride out fee for service or transform to value-based care, this seems to me to clearly be a fee-for-service strategy.
The health care ecosystem is changing and evolving, and we will see significant changes over the next seven years. We are taking this evolution into consideration in our Strategy 2025 planning.
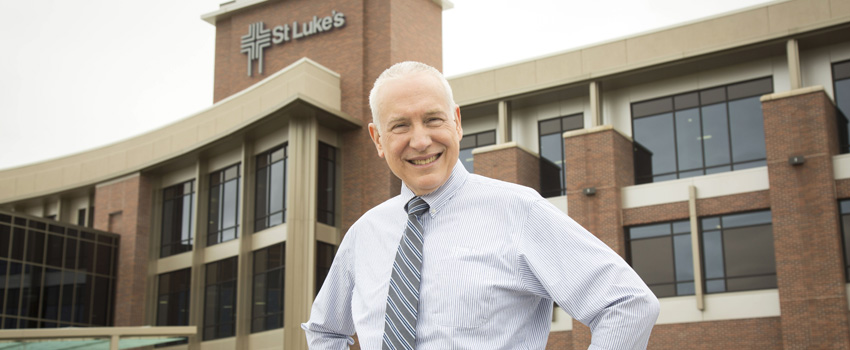
About The Author

David C. Pate, M.D., J.D., previously served as president and CEO of St. Luke's Health System, based in Boise, Idaho. Dr. Pate joined the System in 2009 and retired in 2020. He received his medical degree from Baylor College of Medicine in Houston and his law degree from the University of Houston Law Center.