Dr. Pate’s Prescription for Change
St. Luke’s Care Transition Team Helps Patients Learn How to Live Again

A fragmented health care delivery system results in poor care coordination, excess care, poorer outcomes and much more cost, especially for those patients with multiple chronic diseases.
St. Luke’s care transition program is addressing this problem head on, improving outcomes and lowering the total cost of care in a manner that is very patient-centered.
Here is St. Luke’s Communications Coordinator Chereen Langrill to describe the program and share examples of how it is empowering patients in their health and health care.
- David C. Pate, M.D., J.D.

In the past, 62-year-old Joe Zehanoviz would get so anxious before a doctor’s appointment that he would faint, overwhelmed by the need to manage his conditions and the care of the six different providers he needed to see.
Zehanoviz has chronic heart failure, and his life depends on those provider appointments. But while he received care for his physical condition, his emotional state faltered.
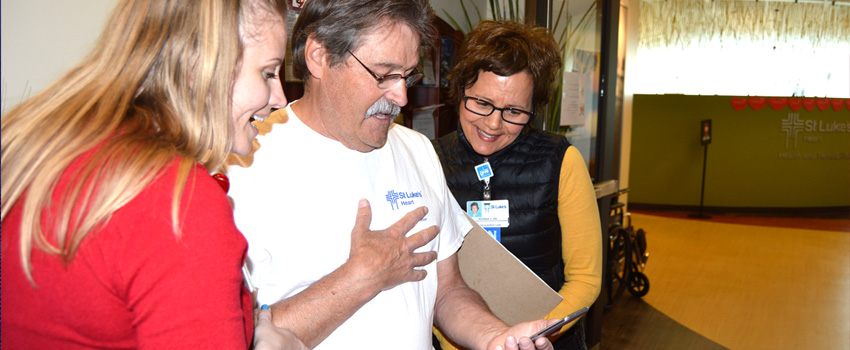
One of his physicians referred him to St. Luke’s Care Transition Program, created five years ago by nurse Linda Mikitish and an advisory committee with representatives from St. Luke’s Heart, Home Care, Quality and Patient Safety and Social Work. The program, within St. Luke’s Heart Health and Rehabilitation program, includes three nurses and one social worker.
After months of work with the team, Zehanoviz is, effectively, a new man. He hopes to buy a home in Middleton soon and feels so good that he plans to do most of his own renovation work.
“Because of the education I’ve had, I am learning how to live again,” he said. “Without that education, I am a dead guy.”
Patients in the Care Transition Program have chronic heart failure, COPD or coronary artery disease. Many have all three conditions, said Pat Lara, St. Luke’s Heart Health and Rehabilitation program director.
Because they are chronically ill or manage multiple health conditions, they make frequent trips to the emergency department. Their care is costly, and they live with chronic pain and discomfort because they are unsure where to go for support or help.
Statistics from the Department of Health and Human Services and multiple other agencies have shown that 5 percent of Americans account for half the country’s medical spending, and it is this complex population – which is more likely to experience multiple hospital admissions and emergency room visits – that providers have begun to focus on as patients, hospitals, insurers and virtually everyone else feels the pain of care costs. The St. Luke’s program’s goal is to minimize those visits and help patients have a better quality of life.
The team often refers to Maslow’s hierarchy of needs, which identifies the five basic areas a human needs to address to be fulfilled. The most basic need is survival (getting enough food to eat, staying warm or having a home). When those basic needs aren’t met, according to Maslow’s theory, it is impossible to move on and meet other needs.
In the case of patients with complex needs, barriers often prevent them from getting the care they need. When barriers block patients from receiving care, the Care Transition team comes in to help.
The team knows, for example, that a care plan is meaningless for someone who doesn’t have money to pay for gas or is feeling too ill to get to a provider’s office for a scheduled visit. If transportation is an issue, they help find rides. Members of the team accompany patients to provider appointments and meet with the patient to recap appointment details. They act as a bridge between patient and provider, explaining the “why” behind recommendations and becoming support systems and resources.
“This is very high-intensity care coordination,” Lara said.
The team works to untangle the knots that disrupt good care, removes barriers to care and sleuths to find answers to ensure care is coordinated and delivered.
Some examples:
- The team helps patients understand why specific treatments or medications are needed so they understand why they need to follow their care plan. Dr. Jennifer Shalz, director of the St. Luke’s Heart Health and Rehabilitation program, hand-wrote a list of the nine medications Zehanoviz was taking and the purpose for each medication to motivate him to take them as prescribed.
- St. Luke’s social worker Mandy Helsley connected Zehanoviz with local philanthropic organizations that could pay his rent and utility bills for one month. That support enabled him to focus on his care plan during a time when his income was limited because of lost work.
- A patient on a low sodium diet might think they are eating the right foods because their meals contain vegetables and lean sources of protein. The team member will check the cupboards, refrigerator and freezer to see what types of foods the patient is eating. Often they find pasta sauce, canned food and frozen meals, items high in sodium. This leads to a discussion about how to choose and prepare healthier foods.
- Patients might not show up for provider appointments because they can’t afford gas or public transportation and don’t have friends or family members who can drive them to appointments. “When a patient runs out of gas, he just doesn’t go anywhere,” Mikitish said. Team members provide gas cards or connect patients with free ride programs offered through community partners.
In a case Lara described as the program’s most extreme example, care coordination saved $500,000. The patient, a 58-year-old man, had multiple chronic conditions. In 2014, he had two emergency department visits, eight hospital admissions and 45 provider visits. The cost of his care was $755,725.
The Care Transition team began working with the patient in 2015, resulting in just one emergency department visit, three hospital admissions and 36 provider visits; the cost of his care that year was $256,367.
Seemingly small adjustments can significantly improve a patient’s quality of life. Helsley worked with Zehanoviz to soften his self-described Type A tendencies that often increase his anxiety and stress level. With her help and encouragement, he has changed the way he cleans his house, and resists the urge to try to achieve spotless perfection.
“She got me to realize how much stress I put on myself,” Zehanoviz said. “I am one of the most detailed people you’ll ever see. She made me realize I don’t need to be that way all the time.”
About The Author

Chereen Langrill was formerly a communications coordinator for St. Luke’s Health System.

