Dr. Pate’s Prescription for Change
Access, Stigma and the State of Research Hinder Help

In last week’s post, St. Luke’s Dr. Kathryn Beattie recounted her family’s heartbreaking struggle for more than a decade to successfully address care needs for her son, who died in the fall following an overdose.
Jack Beattie faced his interconnected mental health and substance abuse challenges in Seattle and at care settings across the country, but hundreds of Idahoans face the same daunting problems. Access for younger people, when detection and treatment can head off a lifetime of woes and costs, is an even greater challenge.
Here, Dr. Beattie follows her powerful writing from last week with steps being taken to address the unmet needs.
- David C. Pate, M.D., J.D.

Community Health Needs Assessments published by St. Luke’s in September 2016 identified improving mental health and reducing suicide and substance abuse among the top three community health needs in all communities served by our organization.
These are recommendations I wholeheartedly support, professionally as a pediatrician and administrator for St. Luke’s Children’s Hospital and personally, as a mom still recovering from the death of my son, Jack, at the age of 20 after his extended battle with mental health and substance abuse disorders.
Psychiatric illness and addiction are often treated separately, but I believe an integrated approach is needed to foster improved outcomes for the many individuals who, like Jack, experience both diseases.
I would like to focus attention on the main obstacles we need to overcome to improve mental health care for our kids: poor access to pediatric mental health expertise; inadequate knowledge and understanding of the science behind mental health diseases; a lack of treatment options for addiction in adolescents and the global lack of coordination between treatment of mental health disorders and addiction, despite the staggering frequency of their co-occurrence; and the stigma of mental health illness, which can result in delayed recognition and thus delayed diagnosis of illness, as well as a delayed willingness of patients and families to seek and accept treatment.
My hope is that sharing Jack’s story in relationship to these obstacles can contribute to lessening the stigma associated with psychiatric illness and addiction, a necessary precursor to a more universal application of an integrated approach for treatment.
Access
Although Jack’s story did not play out in Idaho, it certainly could have. The rate of any mental illness in adult Idahoans is 20.3 percent (2015), significantly higher than the U.S. average of 17.9 percent. Roughly 59,000 Idahoans suffer from serious mental illnesses that cause an inability to function day-to-day, such as a psychotic or serious mood or anxiety disorder.
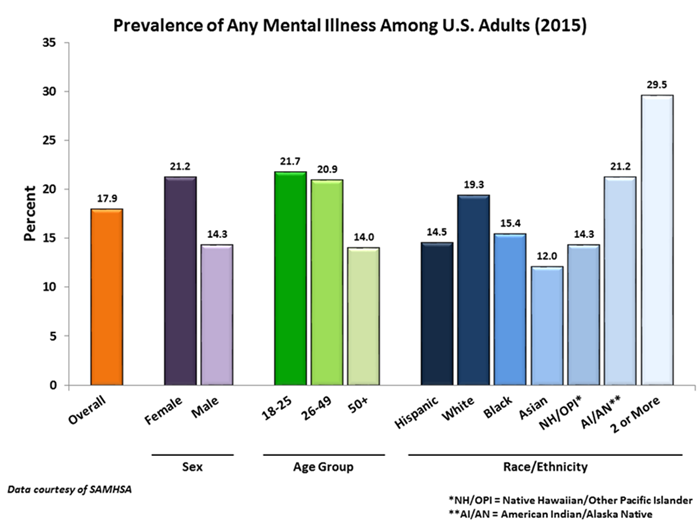
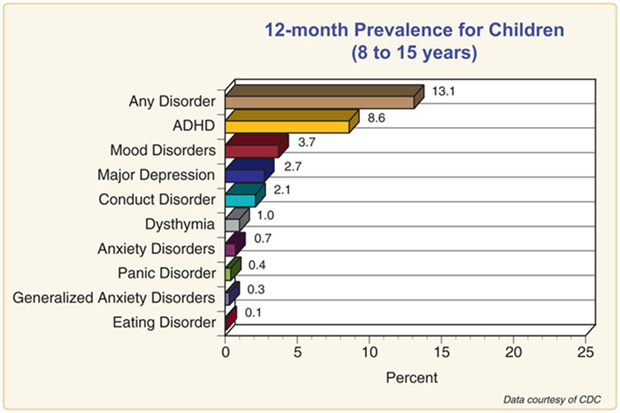
Mental Illness often strikes early in life, so it is common in children. In fact, half of all mental illness emerges by the age of 14 and three quarters by age 24. Research shows that early identification and intervention can prevent mental health crises and prepare children to thrive. Unfortunately, one in seven American youth lives with a mental health condition, but less than half receive any services.
Suicide is the second-leading-cause of death for Idahoans ages 10 to 44, and the overall incidence of suicide in Idaho, at 19 per 100,000 residents, is 46 percent higher than the national average.
Despite these statistics, Idaho is ranked last in the nation for availability of psychiatric care. There is one psychiatrist per 15,676 residents in Idaho; one per 10,000 residents is considered adequate for access to diagnosis and treatment of the population.
At 5.2 psychiatrists and 10.7 psychologists per 100,000 residents, Ada and Canyon counties rank as the lowest in the United States (the average is 11 psychiatrists and 30.7 psychologists per 100,000 residents).
Pediatric psychiatric expertise in Idaho is even more scarce. An extensive search of the Idaho Board of Medicine surfaced only 20 actively licensed child and adolescent psychiatrists practicing in Idaho, which equates to 4.2 child and adolescent psychiatrists per 100,000 Idahoans under the age of 18, or one per 22,049 children/adolescents.
Idaho recognizes the need to improve mental health services and has increased the state budget for the Mental Health Services Department in each of the past three years, making ours one of only 12 states in the country to do so.
To address the shortage, Dr. Sam Pullen, St. Luke’s Health System’s medical director of mental and behavioral health services, has brought The REACH Institute program for patient-centered mental health in pediatric primary care to Idaho.
Conducted as an intensive, in-person, three-day interactive course followed by a six-month case-based distance learning program, this “mini-fellowship” educates pediatricians, family physicians, physicians’ assistants, nurse practitioners, neurologists and psychiatrists in the most current information regarding assessment instruments for diagnosis of mental and behavioral health conditions. Its scope includes the use of psychiatric medications for children and adolescents and educational materials for patients and families. The program supports primary care providers in providing mental health care, expanding availability of diagnosis and treatment.
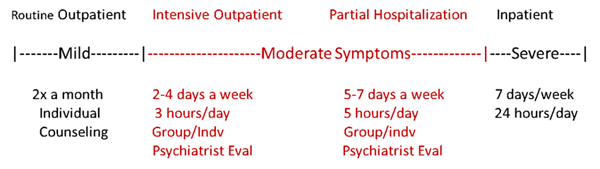
St. Luke’s Children’s is actively recruiting to add two child and adolescent psychiatrists to our medical staff now and planning for more next year. Three additional full-time providers would be an increase of 15 percent in the state. These providers will reserve a portion of their clinic day to provide phone consultation services to primary care providers and will develop services for a continuum of care currently unavailable in Idaho. Today, only routine outpatient counseling and inpatient psychiatry care are available, and these two extremes are often too much or too little care for many patients.
In the fall of 2017, St. Luke’s Children’s will open a partial hospitalization program to provide five to six hours of therapeutic services, five to seven days a week, for a course of two to six weeks as indicated, to stabilize patients following a new diagnosis or acute crisis. Adolescents in a partial hospitalization program will be supported academically and will have the benefit of being at home with family at night for support.
The next step will be to establish an intensive outpatient program for children and adolescents who are ready to return to their regular peer environments. Such programs run three hours a day for two to four days per week after school or work.
With these new programs, patients will have improved options to augment outpatient services or shorten or avoid inpatient psychiatric hospitalization.
Diagnosis
Research into mental health disorders is decades behind the diagnostic and treatment advances of other diseases such as heart disease and cancer. Recently though, increased recognition of the impact of disability caused by mental illness as measured by years lived with disability (YLD) has led to an updated strategic plan by the National Institutes of Health with increased funding for mental health conditions – specifically directed toward early identification and suicide prevention.
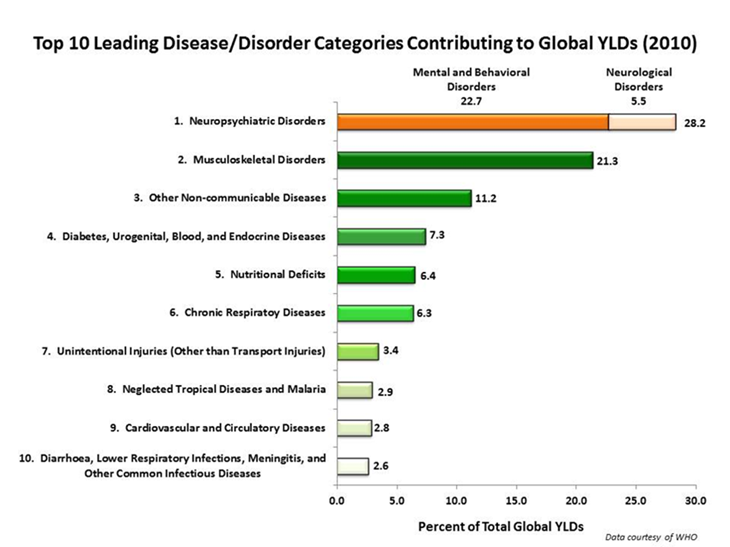
With improved funding, researchers are beginning to identify some of the answers to the underlying cause of both psychiatric illness and addiction in genetics.
For example, scientists have identified gene mutations that impact the transporter function of key neurotransmitters responsible for mood that are linked to an individual being more susceptible to becoming depressed or exhibiting symptoms of PTSD when stressed.
In other words, a depressed patient’s symptoms may be predisposed by genetics and then become manifest with stressors in the environment. Ultimately, we are learning that illnesses such as depression and bipolar and substance abuse are biological in nature, just as are cancer and heart disease – which also result from a combination of genetic and environmental factors. It is simply a matter of identifying the relevant molecules.
But the science of mental health and addiction is much more complex than the expression of just one or two genes impacting brain function, and much more research is needed to find the causes to support earlier diagnosis and develop treatment options.
Genetic research exploring the origins of mental health disorders is a very new science. The Psychiatric Genomics Consortium (PGC), which began in 2007, unites investigators from around the world to conduct meta- and mega-analyses of genomic data for psychiatric disorders, and supports separate workgroups for autism, ADHD, PTSD, bipolar, major depression, OCD and Tourette syndrome, eating disorders, schizophrenia and substance use disorders. The Mayo Clinic is in the midst of a three-year project to collect a “biobank” of the DNA from 2,000 patients with bipolar type I or II to create a data library to make it easier for scientists to explore the genetics of bipolar disorder. The critical research is happening now.
To bring the opportunity for participation in this pivotal research to Idaho, St. Luke’s research department and mental and behavioral health services teams are connected with Dr. Jon McClellan’s genetics lab at University of Washington, which is studying the genetics of early-onset psychosis as well as sporadic schizophrenia and bipolar disorder with psychosis. This will allow our patients and their families to be part of the research that unlocks answers for early diagnosis and improved treatment.
Stigma
The final critical requirement for improving mental health care is elimination of the stigma associated with psychiatric illnesses and addiction. Mental health stigma is multifaceted and encompasses social stigma, the prejudice and discrimination directed towards individuals with mental health disorders; self-stigma (or perceived stigma), the shame and fear of rejection or failure that a patient internalizes as a result of misconceptions about their disease; and structural stigma, the stigma incorporated into social and institutional policies and practices that presents additional large-scale barriers to mental health care.
The misconception that mental health can be controlled consciously has persisted, but the biological basis of mental illness and addiction helps to explain why these patients need much more than good intentions or stronger willpower to overcome their illnesses.
Patients with mental health diseases have been treated differently across societies throughout history, and the misguided view that people with mental health issues are all dangerous, violent, unpredictable, responsible for their illness or generally incompetent is often propagated by social institutions.
In medicine, the separation of mental health care from physical health care, and the lack of parity between coverage for mental health and other health care, also makes it more challenging for patients to access treatment and further promotes the perception that mental health disease is not on the same level as other, more testable and tangible, diagnoses.
Why does stigma matter?
Stigma makes it less likely for a disease to be of interest for funding of research or services. As highlighted above, the National Institutes of Health and the state of Idaho are now driven by data to overcome the bias of this stigma and invest in mental health. But when was the last time you, or anyone you know, participated in a walk or fundraiser dedicated to funding depression, anxiety, suicide or addiction research or treatment? Remember that one in five Idahoans suffers from mental illness, and the number of Americans who die each year from suicide and breast cancer is nearly equal (approximately 40,000 deaths per year). Those who are impacted by either should have hope for treatment.
Stigma makes it less likely for an individual to be transparent about symptoms of the disease because of the negative social implications of having that label if diagnosed.
And once a patient is diagnosed, social stigma makes it less likely that the individual will seek appropriate treatment for fear of being ostracized for having a mental health disease. The belief that psychiatric disease and addiction are manifestations of weakness of character increases the possibility that the patient will believe that appropriate treatment is of no value to them, either due to lack of understanding of the science or a poor sense of self-worth.
The Behavioral Health in Primary Care (BHIP) program is one way that St. Luke’s Clinic is trying to overcome the barriers of stigma. This program places mental health professionals in family medicine and pediatric offices so that a trip to a separate location for mental health care is not required and the collaboration between providers is enhanced.
St. Luke’s providers routinely screen for depression risk at every visit, and referral to an in-clinic mental health resource is frequently a seamless first step for initial evaluation and treatment options for a patient identified at risk.
A caring patient-centered culture, enhanced understanding through well-funded scientific research, improved prevention and treatment options, and supportive social networks can help to overcome stigma and improve early diagnosis and effective treatment of mental health disorders and addiction.
Drug Abuse, Overdose and St. Luke’s Solutions

As we have seen from the outpouring of response to Dr. Kathryn Beattie’s writing last week, many families in our communities have been touched by drug abuse or addiction. Addiction is a powerful, terrible disease, and abuse is a growing epidemic. Far too often, healthcare providers unintentionally contribute to the problem.
At St. Luke’s, we are taking on the problems of addiction and abuse. Here is Dr. Beattie to tell you some of the steps we are taking.
- David C. Pate, M.D., J.D.
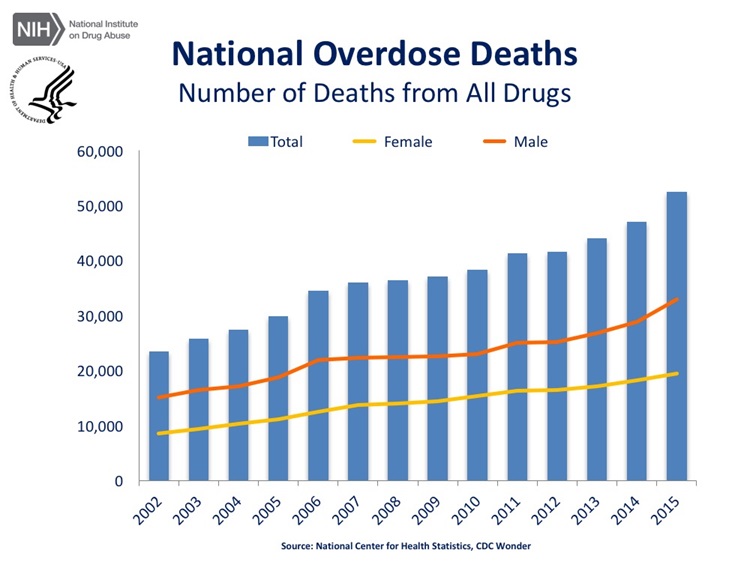
The United States is experiencing an epidemic of drug overdose deaths. The incidence of death involving any type of opioid overdose increased by more than 300 percent between 1999 and 2015; according to the Centers for Disease Control, more than 52,000 Americans died of an overdose in 2015. That is one death every 10 minutes, and of them, 33,000 were related to opioids.
Opioids are a class of drugs that include the illicit drug heroin as well as the prescription pain relievers oxycodone, hydrocodone, codeine, morphine and fentanyl.
Of the 20.5 million Americans 12 or older that had a substance use disorder in 2015, 2 million had a substance use disorder involving prescription pain relievers (an opioid), and 591,000 had a substance use disorder involving heroin. And because substance abuse disorders are believed to have a genetic component, and the risk of opioid addiction increases with exposure, there are reasons to be extremely concerned about the spread of the opioid problem.
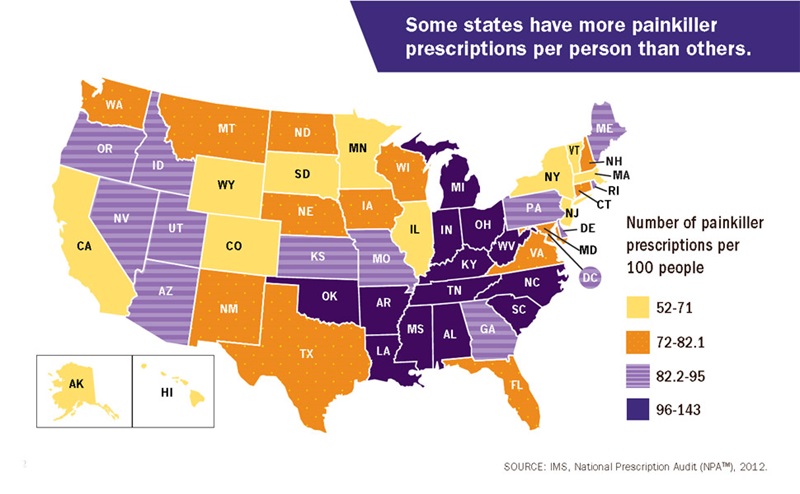
In 2014, more than 240 million prescriptions were written for prescription opioids, more than enough for every American adult to have their own bottle of pills. Four out of five heroin users started out by misusing prescription opioids.
The U.S. Department of Health and Human Services has developed fact sheets about the opioid crisis. And to learn more about how Idaho stacks up, see the National Safety Council’s “Prescription Nation” report.
Healthcare providers must be part of the solution. Opioids have their place in pain management but are not always required, and research is showing that at times, a non-opioid alternative will provide equivalent or better pain control.
A 2009 study published in the Annals of Emergency Medicine demonstrated that pain relief for patients with a broken arm was better with ibuprofen (the ingredient in Motrin and Advil) than with Tylenol with codeine (an opioid). More recent studies in patients following joint replacement demonstrate a reduced need for opiates with the timely use of acetaminophen (Tylenol) post-operatively. Patients are well-advised to ask their physicians if a non-opioid pain medication may be a better first alternative when pain relief is needed, and medical professionals who prescribe pain medications must limit the use of opioids for their patients.
Mandatory prescriber education, opioid prescribing guidelines and prescription-drug monitoring programs have been implemented in many states to enforce smarter prescribing patterns by providers. In Idaho, we are lagging behind. The retail distribution of oxycodone per 100,000 people between 2011 and 2015 increased by 27 percent, from 13,394 prescriptions to 17,013 prescriptions, compared with a national decrease of 9.4 percent during that same time period.
The drug-induced mortality rate in Idaho increased 12 percent between 2011 and 2015, going from 12.6 to 14.1 per 100,000 residents. In a February 2016 Idaho Statesman article titled, “Idaho faces ‘heroin tsunami’ amid opioid abuse epidemic,” Post Falls Police Chief Scot Haug asserted that heroin had surpassed methamphetamine as the most common drug behind marijuana in his community.
The drug use in our region that precedes the deaths is an alarming harbinger of what is to come; St. Luke’s Community Health Needs Assessments have found that the percent of people who report using illicit drugs in our communities is more than twice as high as Idaho as a whole.
This is not “someone else’s problem.” This is a problem in our communities.
Four in five new heroin users started out misusing prescription painkillers. The rate at which prescriptions for opioids are written for adolescents and young adults has doubled in the past 20 years, which is alarming. Even more alarming: Most adolescents who misuse prescription pain relievers are given them for free by a friend or relative or have taken them from a stash of leftover medication in the medicine cabinet.
St. Luke’s serves as a drop-off point for community members to leave outdated and no-longer-needed prescription drugs to remove them from homes and away from teens. Between January and September of 2015, in partnership with the Meridian Police Department, we removed 2,100 lbs. of drugs from the Meridian community alone, and we have been awarded a grant from the Office of Drug Policy to extend this program for youth in the rural areas of Fruitland, Payette and Weiser.
April 29 is 2017 National Drug Take-Back Day. Please clean out your medicine cabinets and take unused medications – yours and your pets’ – to a local drop-off center.
At St. Luke’s Children’s, we are addressing drug use/abuse among our preteen/teenage population through our Prescription Drugs: Let’s Talk about It program. This program provides education opportunities in the form of a toolkit, community outreach during school registration and social media.
Adolescents and people with mental disorders are at a greater risk of drug abuse and addiction than the general population. The co-occurrence of chemical dependency/substance abuse disorders and a mental health diagnosis is close to 50 percent, yet most care facilities separate the treatment of the two. This high rate of co-morbidity would indicate the need for a comprehensive approach to intervention that identifies and evaluates each disorder for development of a concurrent treatment plan.
In Idaho, we need to increase the availability of medication-assisted treatment facilities for opioid addiction and improve coordination of care for patients with co-occurring disorders. St. Luke’s and St. Luke’s Children’s look forward to working with our community partners to identify better ways to reduce access to prescription medications, educate our patients to prevent non-medical use of pain relievers and reduce substance abuse, and deliver coordinated substance abuse treatment and mental health care to meet community needs.
About The Author

Dr. Kathryn Beattie is the executive medical director of St. Luke’s Children’s Services.



