St. Luke’s Newsroom
When people thrive, communities grow stronger. Explore stories highlighting how St. Luke’s supports our patients, neighbors and communities, collaborates with nonprofit organizations to improve health, and celebrates team members, partnerships and milestones.
Featured Articles

Community Health & Engagement
All in the family: Mom, son, daughter team up to serve patients in St. Luke’s Elmore operating roomsIt is one thing to have a work environment that would be described as a “family atmosphere.” In the operating rooms at St. Luke’s Elmore, it is literal.

Community Health & Engagement
Improving access to care: COMPASS honors partnership to boost patient transportationSt. Luke’s in recent years has worked with local organizations to broaden eligibility for transportation assistance.

Patient Care
Emerging Technologies Lab helps St. Luke’s stay on the cutting edge — with smart decisionsThe lab opened in October 2025 with the mission of creating a space where St. Luke’s staff members could evaluate new technology and explore different workplace solutions.

Community Health & Engagement
How St. Luke’s and a community partnership helped create ‘home away from home’ for recovering patientSt. Luke’s partners with the community to create a safe place for healing.
Read more News & Announcements from St. Luke’s
View all
Patient Stories
Meet Maddie: Children’s Miracle Network champion ‘super woman’ thanks St. Luke’s care, inspired to become nurseSometimes, the smallest among us can provide us the biggest show of strength and perseverance.

Community Health & Engagement
All in the family: Mom, son, daughter team up to serve patients in St. Luke’s Elmore operating roomsIt is one thing to have a work environment that would be described as a “family atmosphere.” In the operating rooms at St. Luke’s Elmore, it is literal.

Community Health & Engagement
Improving access to care: COMPASS honors partnership to boost patient transportationSt. Luke’s in recent years has worked with local organizations to broaden eligibility for transportation assistance.

Patient Care
Emerging Technologies Lab helps St. Luke’s stay on the cutting edge — with smart decisionsThe lab opened in October 2025 with the mission of creating a space where St. Luke’s staff members could evaluate new technology and explore different workplace solutions.

Community Health & Engagement
How St. Luke’s and a community partnership helped create ‘home away from home’ for recovering patientSt. Luke’s partners with the community to create a safe place for healing.
Read more News & Announcements from St. Luke’s
View allAdvancing Community Health

Community Health & Engagement All in the family: Mom, son, daughter team up to serve patients in St. Luke’s Elmore operating rooms
It is one thing to have a work environment that would be described as a “family atmosphere.” In the operating rooms at St. Luke’s Elmore, it is literal.

Community Health & Engagement Improving access to care: COMPASS honors partnership to boost patient transportation
St. Luke’s in recent years has worked with local organizations to broaden eligibility for transportation assistance.

Community Health & Engagement How St. Luke’s and a community partnership helped create ‘home away from home’ for recovering patient
St. Luke’s partners with the community to create a safe place for healing.
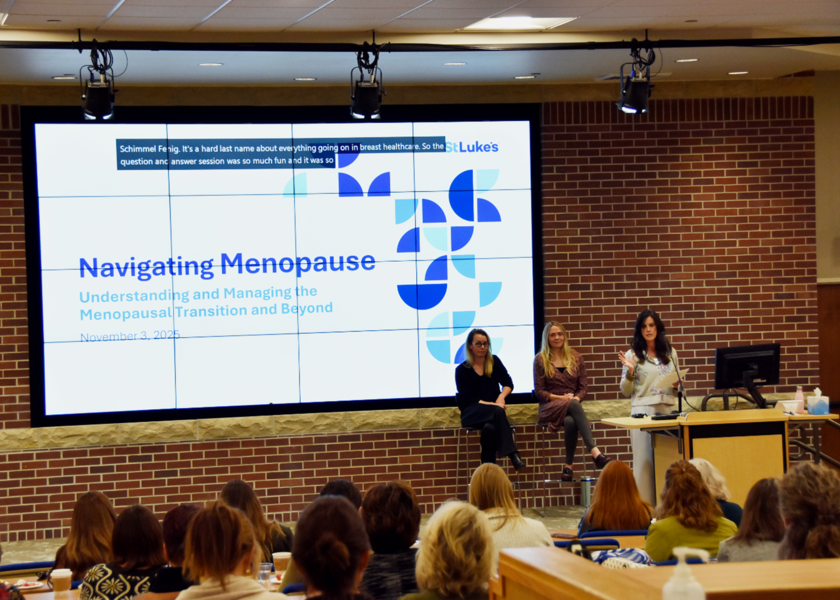
Community Health & Engagement St. Luke’s Women’s Forum empowers important health conversations in the Treasure Valley
What started as a simple idea has evolved into a gathering where hundreds of women have found comfort in sharing their stories and concerns.

PATIENT STORIES
While enduring multiple surgeries and intensive treatments for two bouts of cancer at St. Luke’s Children’s, Maddie’s determination never wavered. Now in recovery and continuing follow up care, she looks ahead with resilience.
St. Luke’s 2026 Children’s Miracle Network Champion, Maddie




