Community Health & Engagement
Twin Falls Chamber of Commerce gets up close stroke training from St. Luke’s team
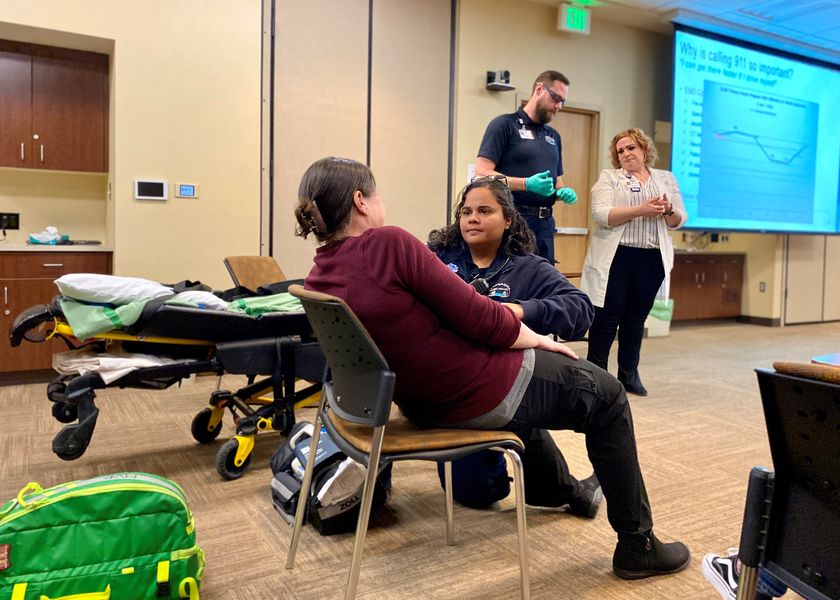
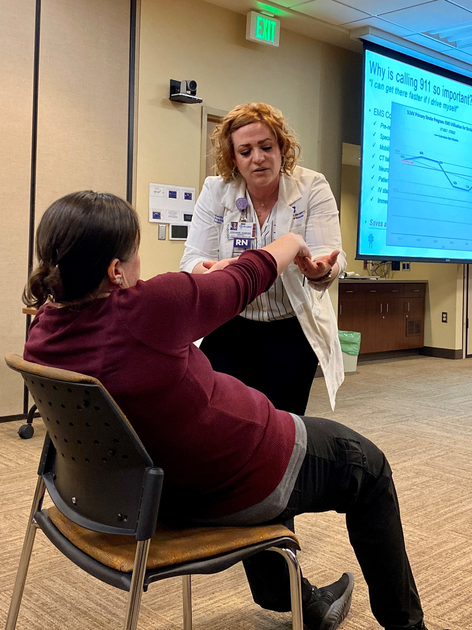
The training’s mock patient gets checked out by St. Luke’s team members.
By Kelly FransonLast Updated March 16, 2023
Recognizing the signs of a stroke is an important lesson for any audience, but a Twin Falls Chamber of Commerce leadership group was recently treated to an eye-opening demonstration of life-saving skills at St. Luke’s Magic Valley.
The presentation started like any other, with Stephanie Shawver, stroke program manager for St. Luke;s Magic Valley, Jerome and Wood River, leading the group through a presentation on stroke recognition.
Toward the conclusion of the presentation, a member of the St. Luke’s Magic Valley SIM lab team that was planted in the audience pretended to suddenly develop stroke symptoms.

Presenting to the Twin Falls Chamber of Commerce group.
“This is not real, it is a planned demonstration for you,” Shawver announced before guiding the Chamber of Commerce group through a real-time BE FAST assessment while another St. Luke’s SIM team member, Michelle Eberle, was sent to “dial 911.”
A Magic Valley Paramedics crew staged outside the conference room “responded” to the simulated emergency. The crew walked the audience through the EMS Code Stroke process, which includes IV starts, lab draws, in-field lab testing, a specialized neurologic assessment and notification of the emergency department physician and teams.
The EMS process is designed to fast-track patient care (with scene times of 10 minutes or less) by performing many of the tasks that normally occur after arrival to the emergency department. This allows the patient to seamlessly transition directly to CT scan upon arrival and ultimately speeds up treatment by an average of 13 minutes.
The specialized neurologic assessment performed by EMS not only confirms stroke as a likely diagnosis but also identifies large vessel occlusion stroke, a type of stroke requiring a time-sensitive procedure performed at only three Idaho hospitals, the closest being St. Luke’s Boise.
If the assessment is positive for suspected large vessel occlusion stroke, Air St. Luke’s is placed on standby in the emergency department, prepared to transfer the patient as soon as the diagnosis is confirmed on CT. This innovative solution saves an average of 60 minutes on time to definitive treatment and has received national attention as an emerging best practice in rural settings.